activation
▼activating agents : B cell activation : costimulatory agents : costimulatory cells : complement activation pathways : dendritic cell activation : granulocyte activation : lymphocyte activation : macrophage alternative : macrophage classical : markers : mediators : monocyte-macrophage : pDC : phagocyte activation : precursor dendritic cells : signaling/receptors : T cell activation : Tc activation : Th activation▼
Activating agents
_ ● antigen
___ ● pathogens
___ ● pathogen-associated molecular patterns (PAMP)
___ ● danger-associated molecular patterns (DAMP)
Markers
___ ● major histocompatibility complex (MHC) molecules
Costimulatory agents
___ ● CD28
___ ● SLAM (signaling lymphocytic activation molecule), a 70-kDa costimulatory molecule belonging to the Ig superfamily
___ ● ICOS (inducible costimulator) molecules
___ ● TNFR: CD40, CD30, CD27, OX-40, 4-1BB
___ ● negative regulators of costimulation: CTLA-4, PD-1
Costimulatory cells
● helper T cells (Th) for activation of B cells, and APCs for activation of T cells
_ ●Antigen presenting cells display epitope proteins – exogenous antigen or fragmented angtigen from phagocytosed cells – on their surfaces. APCs include:
___ ● phagocytic cells – dendritic cells, macrophages
___ ● B cells (B lymphocytes)
Signaling / receptors
_ ● pattern recognition receptors
_____ ● complement receptors (table)
_____ ● Fc receptors (table)
_____ ● scavenger receptors (table)
_____ ● Toll-like receptors (table)
_ ● TNFR
_ ● B cell receptors (BCR)
___ ● immunoglobulin - antibodies (table)
_ ● T cell receptors (TCR)
_____ ● clusters of differentiation
_____ ● major histocompatibility complex (MHC) molecules
Mediators
_ ● immune cytokines (table)
Phagocytes
Dendritic cells
Dendritic cells and their immature counterparts, Langerhans cells (LC), are highly specialized, professional antigen-presenting cells (APC). Immature dendritic cells are called 'veiled cells' because they display large cytoplasmic 'veils' rather than the long dendritic projections of mature cells. As key regulators of immune responses, dendritic cells (DC) stimulate lymphocytes to perform cell-mediated and humoral immune responses against pathogens and tumor cells.
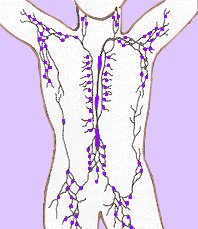
Immature, precursor dendritic cells (pDC) circulate throughout the body, migrating to lymphocyte rich tissues (such as spleen and lymph nodes) upon stimulating encounter with antigen. The dendritic cells internalize the antigen then externalize (fragmented) antigen that they present to lymphocytes in MHC-peptide complexes, expressing markers that stimulate lymphocyte activation.
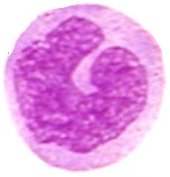
Monocyte → macrophage activation
Production of the macrophage lineage from progenitors in the bone marrow is typically controlled by M-CSF, which is constitutively expressed by many cell types. Serum levels of M-CSF and GM-CSF increase in response to invasive stimuli and inflammation, and monocyte numbers increase dramatically. M-CSF-derived macrophages are larger, and have a higher phagocytic capacity, while GM-CSF-derived macrophages are more cytotoxic against TNF-α-resistant tumour targets, express more MHC class II antigen, and constitutively secrete more PGE-2.
Classically activated macrophages are associated with chronic inflammation and tissue injury wherein classically activated macrophages exhibit a Th1-like phenotype, promoting inflammation, destruction of the extracellular matrix (ECM), and apoptosis. Classical macrophage activation proceeds in two stages.
1. IFN-γ-primed stage in which macrophages exhibit enhanced MHC class II expression, antigen presentation, but reduced proliferative capacity. (IFN-α, IFN-β, IL-3, M-CSF, GM-CSF and TNF-α can also prime macrophages for selected functions.)
2. Secondary stimuli operated to fully activate primed macrophages. Diverse agents provide secondary signals (including LPS (CD14), bacteria, yeast glucans, GM-CSF and phorbol esters). Macrophages stimulated for tumoricidal activity secrete IL-1, display decreased MHC class II gene transcription, and are generally poor antigen presenters of antigen.[r]
Alternatively activated macrophages typically resolve inflammation and facilitate wound healing wherein they display a Th2-like phenotype, promoting construction of ECM, cell proliferation, and angiogenesis. Alternative macrophage activation does not require a priming stage and IL-42 and/or IL-1326 can act as sufficient stimuli.[r2]
Granulocyte activation
The hematopoietic cytokines, granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) have pleiotropic activating effects on mature leukocytes, which can improve leukocyte function, facilitating eradication of microbial infections. G-CSF activates neutrophils, while GM-CSF activates neutrophils, eosinophils, and monocyte/macrophages.
Lymphocytes
B cell activation: naïve B cells → plasma cells
Activation of naïve B cells occurs when a BCR (antibody) encounters and ligates its cognate antigen. B cells are coated in immunoglobulin receptors and are able to recognize intact antigen, which they engulf, digest, and subsequently present in complex with surface MHC class II molecules. The MHC-peptide complex binds CD4 + helper T cells (Th), inducing secretion of cytokines that stimulate B cell proliferation and their differentiation into plasma cells, which secrete specific antibodies that bind with the cognate antigen. These antigen-antibody complexes are subsequently cleared by liver and spleen cells and the classical complement cascade.
T cell activation:
Activation of T cells requires a first signal of TCR engagement, which ensures antigen specificity and MHC restriction of the response. The second signal comprises synergistic costimulatory signaling by professional antigen presenting cells. The costimulatory second signal is necessary to sustain and integrate TCR signaling to stimulate optimal T cell proliferation and differentiation. The level of activation of T cells is closely related to their state of differentiation.
Activation of the resting Tc cell involves two steps: 1) TCR on the CD8+ cell interacts with antigen-class I MHC complex on the surface of a target cell. 2) CD8+ Tc cell is stimulated by cytokines, particularly IL-2, which have been secreted predominantly by activated Th cells. Resting Tc do not express IL-2 receptors until antigen stimulation increases the expression of Tc IL-2 receptors, ensuring that activation is confined to Tc cells that ligate cognate antigen. Activated Tc cells become CTLs.
The first signal for helper T cell (Th) activation is interaction of the TcR-CD3 complex with antigen-MHC class II molecules on the surface of an antigen presenting cell. Stimulation is aided by the CD4 molecule on Th cells, with or without assistance from other accessory molecules, such as CD45, CD28 and CD2. Increased IL-2 secretion by the T cell and an increase in IL-2 receptors on the T cell surface trigger a cascade of biochemical events.
Three pathways are involved in complement activation:
● classical pathway (binding of an antibody to its cognate antigen)
● alternative pathway (relies upon spontaneous conversion of C3 to C3b)
● mannose-binding lectin pathway (MBL -MAPS) (homologous to the classical pathway, but utilizes opsonin, mannan-binding lectin (MBL) and ficolins rather than C1q)
▲ф A activating agents § adaptor protein ~ adhesion molecules ф affinity maturation ♦ AID ф anergy ф antibodies ф antigen ф APCs סּ apoptosis ф autoimmunity B : B cell activation ф B cells ọ blood ọ bone marrow C סּ caspases ф CD סּ cell-cycle control ₪ cellular fate ф cellular response סּ cellular signal transduction סּ chemotaxis ф class-switch recombination ф clonal selection ф complement system : complement activation pathways : costimulatory agents : costimulatory cells ~ cytokines ~ cytokine receptors D סּ death receptor : dendritic cell activation ф dendritic cells ₪ differentiation E סּ ECM F ♦ Fyn G ф gene conversion ọ germinal centers : granulocyte activation ф granulocytes H ф helper T cell ф hematopoiesis ф humoral immunity I ф immune cytokines ф immune response ф immune tolerance ~ immunoglobulins § immunoglobulin isotypes ф inflammatory response ф interferons ф isotype switching L ф leukocytes ф leukocyte adhesion cascade : lymphocyte activation ф lymphocytes ọ lymphoid system ф lymphokines ф lymphoid system M : macrophage alternative : macrophage classical ф macrophages ф MHC ф migration ¤ mitogens ф monocytes : markers : mediators : monocyte-macrophage N § NF-κB P ф pathogens ф pattern-recognition receptors : pDC : phagocyte activation ф phagocyte ф plasma cells : precursor dendritic cells ¤ proliferation R ф receptors S ф secondary antibody diversification ф signaling ¤ signaling molecules : signaling/receptors סּ signal transduction ф somatic hypermutation, somatic mutation ф surface receptors T : T cell activation ф T cells : Tc activation : Th activation ф thymus ọ thymus ф (tolerance) ▲ф
Complement Receptors Fc receptors Immune Cytokines Immunoglobulins Interferons Scavenger Receptors Toll-like Receptors
▲ Top ▲
tags [Immunology] [activation]
Labels: activation, antigens, costimulation, dendritic cells, differentiation, macrophage, maturation, mediators, monocyte, pathogens, phagocytes, precursor, production, proliferation, receptors, signaling
| 0 Guide-Glossary